No products in the cart.
NZDA News Article, Infection Prevention and Control
Getting the foundations in place
‘Keep it simple’ they say… a common recommendation when it comes to approaching the common question “How do I know we’ve got really good infection prevention and control in our practice”?
The real trick to being confidently compliant is managing to simplify what can be a reasonably complex mix of microbiology (infectious cycle), biochemistry (products and how they work) and physics (sterilisation). This can be a great deal more challenging than just “keeping it simple”! In essence, trusting the science gives a strong framework and structure to support the team to understand why they do what they do. The ‘why’ is the everything. Most importantly this removes some of the commonly heard “he said, she said” rhetoric… “We used to do it like this at my old practice”, “I’ve worked in a Govt department, and this is how we did it”… you will have heard it all I don’t doubt.
Compliance is the aim. PPE is the defence, communication and vigilance is the strength.
What we do know is that prevention is the only cure, and that for now infection prevention and control is the best way forward. We have learned to live in a constant state of readiness.
All infection prevention protocols should be based on regulatory body standards and guidelines. However, to be able to feel confident in compliance, infection prevention and control management needs to be supported with strong leadership; fostering and setting an expectation of a team managed approach to be adopted by all team members. And as above, importantly to be kept as simple/ simplified as possible.
Infection prevention foundations are firmly rooted in administration, the development of, and subsequent assessment of robust policies and procedures. Luckily then, most Practice Managers love documents, organisation, policies, procedure manuals, ‘How We’ detailed work instructions, checklists, audits, quality management, and record keeping. Perfect!
Everyday clinical life can be a myriad of planned and unplanned, unexpected events—“one of those days” as we say. There are many, many things to focus on; patients, materials, equipment that is or isn’t working that day, documentation, phone calls, emails, the list is never ending. An unintended consequence of this busyness can be that management of infection prevention can be overlooked or compromised.
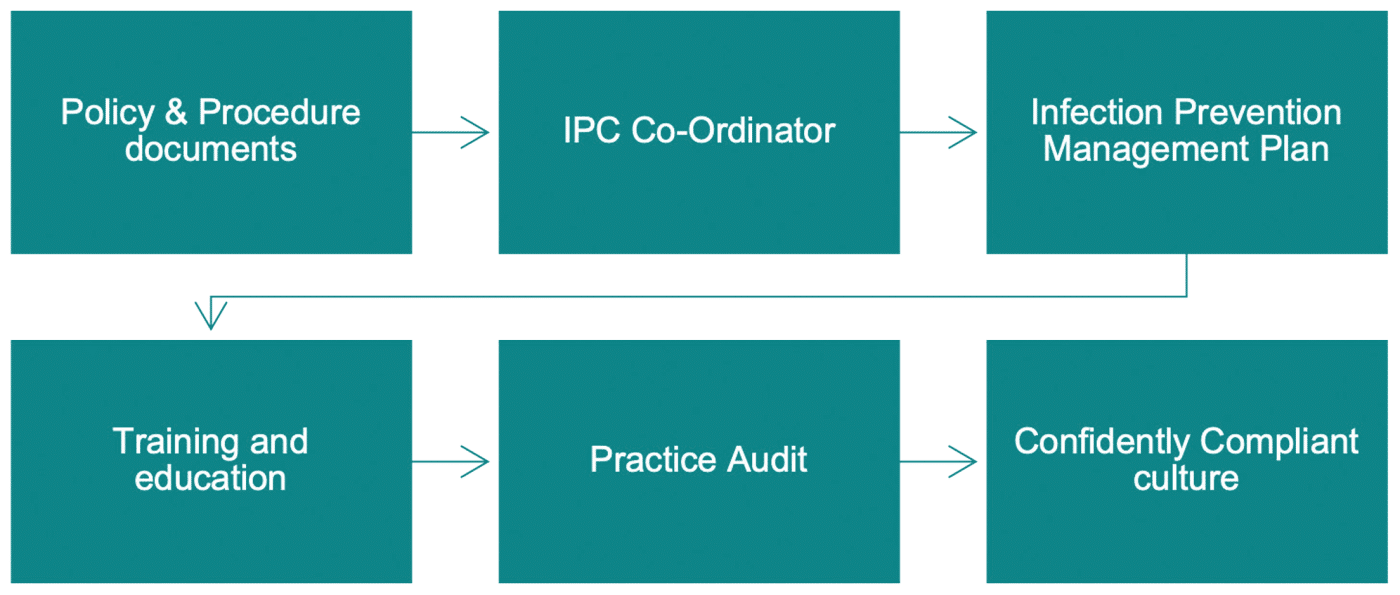
From a practice management perspective, creating and maintaining a strong approach to infection prevention should include the following;
1. Policy and procedure documentation.
Clear policies and procedures that align with relevant standards and industry documents are critical to ensuring compliance. Having specific working instructions removes deliberation as to how tasks are performed.
A Policy and Procedure Manual can be utilised as part of the practice’s new staff induction process and when combined with training, ensures new team members are provided clear information on practice processes. Consolidating processes and products used can support a shift in focus to a team managed approach by involving all team members in the decision making. This helps those not involved clinically to understand the time involved and why specific products might be used. It can empower staff that undertake clinical tasks to align processes and products with requirements for compliance—product rationalisation is always beneficial!
Do you have all necessary documentation required to formulate a comprehensive policy and procedure manual?
Take time to review your policies and procedures—do you have everything documented and have all the team read these? Have they been updated at the time of Performance Requalification (Validation) (PRQ) as necessary?
Have you written up ‘how we do’ things? Do you know where to access these documents?
Documented processes are a regulatory requirement, and as such, are legally imperative. So an important area to focus on administratively. It is a requirement to have both soft and hard copy of Standards and Guidelines accessible to all staff.
These documents give a solid framework to develop a comprehensive risk management strategy for the practice. Robust policies and procedures create the framework for practical tasks but once we get safe how do we stay safe?
2. Appoint an Infection Prevention Co-ordinator—bring the team together and improve compliance outcomes.
While all team members contribute to and support overall infection prevention management, it is recommended to delegate ‘co-ordination’ of all aspects to one/ two people. This may be the Practice Manager or non-clinical team member, with a clinical team member who can work together to hold the team accountable and oversee the practice Infection Prevention Management Plan, reviewing and evaluating processes regularly for compliance. They need to be conscientious in maintaining expected protocols and prepared to raise concerns when necessary (and should be supported when they do).
Working in the clinical environment can highlight potential non-compliance with procedures and present opportunity to consider how something could be improved. For this reason, it is beneficial to have one appointed IPC Co-ordinator with a clinical focus.
Remember, infection prevention is a ‘team game’, even though the practice manager and/or dental assistant have been delegated the responsibility and provided with clear policies and procedures to follow, clinicians and other team members must be held accountable as required.
The IPC Co-ordinator should have a clearly defined job description with these additional responsibilities, have time allocated to undertake these responsibilities, and be trained so they can be knowledgeable and remain up to date with current requirements.
This role is aligned with both the Practice Manager and Principal Dentist so a strong, positive, and proactive approach and communication will be required.
Empower your IPC Co-ordinator to make decisions and changes that reflect best practice infection prevention to maximise the opportunity to Get Safe. Be Safe and Stay Safe.
3. Have an Infection Prevention Management Plan. A documented plan that outlines measures taken to prevent or minimise risk of infection for your patients and staff members, listing risks and how including the measures you have in place are suitable and effective.
The IPMP should contain:
- — Handwashing and hand hygiene
- — Personal protective equipment
- — Management of blood/body fluid exposures
- — Infection prevention and employee health
- — Immunisation
- — Environment management and hygiene
- — Pre-treatment risk assessment
- — Use of single use items and reprocessing of reusable instruments and equipment
- — Delegation of responsibility for infection prevention and control
- — Incident management and reporting
4. Training—implement a staff training schedule for all team members.
Training in some form must be undertaken annually. Ideally training and learning should be ‘continuous’; an ongoing schedule of various aspects planned out over a year to ensure all team members feel updated and in touch with what feels like a never-ending changing landscape. Many staff have commented they feel ‘safer’ when they are updated frequently.
When it comes to providing induction and IPC training to new team members (some who may have not ever have been exposed to dental settings), do you have the time? Provide induction along with Infection Prevention and Control training for your new team members not forgetting the rest of the team IPC annual training. Are you observing a team managed approach with accurate and compliant processes? In other words, is everyone doing the same thing and is the team aligned?
Training that gives an understanding of importance on both how something is done, and why it is done is more likely to achieve compliance with what is being expected to be done, e.g. hand hygiene, standard precautions, transmissionbased precautions, PPE, aerosol management, waterline management, cough etiquette, surface management and sterilisation.
Training can play an important role in team cohesion and help resolve differences if team members disagree about certain processes.
Attending a training session together as a team or having someone come into the practice to train can be a beneficial exercise; everyone hears the same information at the same time. Hearing information from a third party can reinforce the need for alignment of processes and get everyone on the same page. Once the team are updated, training may be undertaken internally by a member of the team.
5. Infection Prevention and Control Audit—what gets measured gets done.
To improve, we need to measure. The first step in developing an effective infection prevention and control system is to identify every point of risk in the dental practice. No shortcuts, if you haven’t done it yet, the practice needs to instigate a formal and comprehensive audit. Use an audit tool (NZDA Toolkit Checkup) or engage an independent consultant. Many practices don’t have the time or resources to do their own audit or want to ensure it is conducted by a skilled specialist for additional peace of mind.
The ‘Great Reshuffle’ it has been called—moving to a new career, change of focus, interest, resulting in many practices finding themselves employing staff without dental background or experience. It’s a positive aspect to bring fresh energy into dentistry and we should embrace it.
Crystal clear and well-defined role responsibilities with job descriptions and providing infection prevention focused training, are more likely to support compliance. In addition, a skills matrix or competency assessment tool of some kind should be used to assess individual compliance.
Add Compliance as an agenda item to monthly team meetings to keep everyone updated of any changes, or to positively acknowledge excellent level of ongoing IPC management.
This reinforces a commitment to being conscientious in maintaining a confidently compliant approach.
There are varying levels of accountability and responsibility within the dental team for infection prevention and control. The clinician is ultimately accountable for processes undertaken, while practical tasks are delegated with several team members usually taking responsibility for performing them.
Expect and encourage a ‘team huddle’ morning or pre session meeting— preparing for a safe patient visit, with optimised clinical workflow and PPE management discussed between clinician and assistant. It may only require a brief meeting; review of patients records for special patient’s needs (i.e. latex allergy), treatment requirements, set up of instruments, handpieces, supplies, disposable items, prostheses, equipment, availability of necessary PPE, hand hygiene products, sharps management, changeover, added or important points all support a safe and efficient changeover ensuring adequate time is made for, and attention given to suction and waterline management, safe transportation of instruments etc.
‘Walkabout’—complete a walk through the practice, review from the patients’ perspective. Check cleanliness of clinical areas, reception area, windows, desks, and bathrooms. Start at the front door and make certain all areas are clean and tidy. The potential consequences of dust are that microbes can survive in sticky substances on chair arms, in fingerprints and can be carried about on dust particles. This can all lead to disease transmission opportunity and cross contamination. Patients can’t see microbes of course, but they can see smudges, f ingerprints, dust, and cobwebs.
Respiratory Hygiene—‘Cover Your Cough’. Provide tissues, waste bin (lined and lidded), alcohol-based hand rub and a ‘Cover Your Cough’ sign in your reception area to encourage respiratory hygiene and cough etiquette to help reduce the spread of respiratory microbes. Encourage patients to ‘Catch It. Kill It. Bin It’.
‘THINK’ Compliance. Build an Infection Prevention Brand Culture. Behaviours can be the most challenging aspect of maintaining compliance with infection prevention procedures. Having a compliant way of thinking and leading by example promotes team managed infection prevention and control strategies. Being familiar with and understanding practice standards and industry guidelines is a must.
As mentioned, keeping infection prevention procedures simple is important. Implement them effectively by building an infection prevention driven culture— how you ‘do things’. Always at its best when leaders lead by example and employees do the right thing even when nobody is watching. The ‘confidently compliant conscience’ you might say!
Good compliance comes from the flow on effect of compliant behaviour. The key to this is an engaged, cohesive, team-managed approach to infection prevention and control. Behavioural change, when it comes to infection prevention and control, is one of the most difficult aspects to manage.
It’s always good to be aware. There may be some elements you might recognise in the following ‘staff members’ that could be reflective of your practice. Anyone familiar…?
‘Been There, Done That’ Betty: may be resistant to change and regardless of practice procedures, just does it the way she always has. A classic example of this is manual cleaning (scrubbing) instruments because it ‘does a better job’. Training and giving an explanation of ‘why’ something is required or recommended can be the easiest way to align team members.
‘New Girl’ Nancy: may have come to your practice thinking everything done at her previous practice was correct. This may not be the case and is the very example of why policies and procedures specific to your practice, products and equipment are an absolute must.
‘Practice Manager’ Penny: may be a highly efficient business manager who has never worked clinically. It can be challenging for non-clinical staff to fully understand time required for changeover after patient treatment, manage instruments, set up or close the treatment room, perform sterilisation monitoring or why the team requires specific products for complete testing processes. Having an assigned IPC Co-ordinator who has a clinical focus to work with the practice manager can problem solve this and give great assurance and support to the practice management role.
‘Dental Assistant’ Deb: wants to do the right thing, preferably without causing a stir. She has completed an infection prevention course and has been trying to implement some necessary changes but having trouble getting other team members to listen. She is frustrated the team haven’t all heard the same information, this makes it difficult for her to communicate the message. She will try her best to get everyone on board but decides her knowledge might be put to better use elsewhere and sadly leaves.
The outcome of any element of these behaviours can be a disruption to the practice and make infection prevention procedures less time and cost efficient. It can also lead to non-compliance.
The importance of infection prevention and control as a constant state of readiness for any unexpected health crisis has always been well and truly embedded in our psyche. Perhaps the necessity to document, train, check and assess, have management plans, and continuously promote a team approach has been highlighted.
—
This article originally appeared in Volume 207, March 2022 of NZDA News.



 Coaching Solutions
Coaching Solutions













